FTC Highlights PBMs Mafia-Esque Power Over Patients and Pharmacists
Washington, D.C. — In response to the Federal Trade Commission’s (FTC) latest Interim Staff Report on consolidated pharmacy benefit managers (PBMs), as part of an ongoing 6(b) inquiry announced back in 2022, the American Economic Liberties Project released the following statement.
“The FTC’s interim report highlights a painful reality that’s all too familiar to Main Street pharmacies and patients: PBM giants are ruining U.S. healthcare and must be stopped,” said Benjamin Jolley, PharmD, Senior Fellow for Healthcare at the American Economic Liberties Project. “Not only do the biggest PBMs inflate drug costs and overcharge patients, even for critical medications like cancer drugs, but they also deprive the independent pharmacies many Americans depend on of profit and revenue, killing their businesses. This report is sounding yet another alarm for policymakers and enforcers to crack down on these exploitative middlemen, eliminate the rebate system they abuse, and break their mafia-style control over the pricing and delivery of essential medication. We applaud the FTC for scrutinizing these monopolists, but now encourage the Commission to use its full authority to stop these middlemen and lower drug prices.”
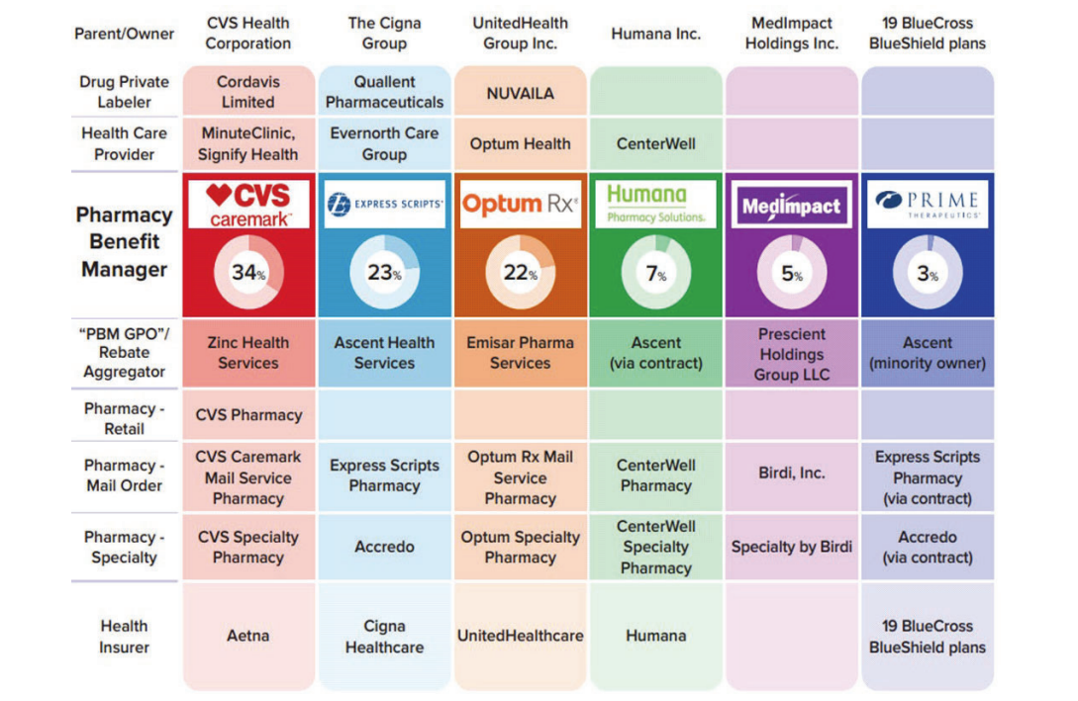
The FTC’s report reveals that the top three PBMs—CVS Caremark, Express Scripts, and OptumRx—now control almost 80% of the 6.6 billion prescriptions filled in the US. Their concentrated power leads to higher drug costs and the shuttering of independent pharmacies, particularly in rural areas where they are often the only healthcare providers. The report also highlights the opaque and unfair contractual practices PBMs impose on pharmacies, which makes it hard for them to survive.
Initially established to process drug claims, PBMs are now sprawling intermediaries between drug manufacturers, insurers, and pharmacies—controlling access to pharmaceuticals through formularies. They prioritize drugs that offer the highest rebates, often sidelining more affordable options like generics. PBMs take a cut of this rebate before passing the remainder on to the insurer. Despite PBMs’ claims that rebates make medications more affordable, they actually incentivize the selection of higher-priced drugs, pushing the cost burden onto patients who pay based on inflated list prices.
PBMs have expanded their influence through vertical integration, merging with health insurers and specialty pharmacies, thereby steering patients to their own affiliated pharmacies and squeezing out competitors. These practices not only harm small businesses but also limit patients’ access to affordable medications. The FTC’s findings call for immediate regulatory and legislative action to ensure that PBMs operate with greater transparency and accountability, in order to protect both consumers and independent pharmacies from their anticompetitive tactics.
All Categories





